Happy New Year! 2021 was a hugely positive year for FASD, gathering yet more momentum for progress. With that in mind, at National FASD we’re starting 2022 with a lot of excitement. It’s important that all families supporting loved ones with FASD understand these changes, as they are tools for us all in the fight for change.
The weight of progress
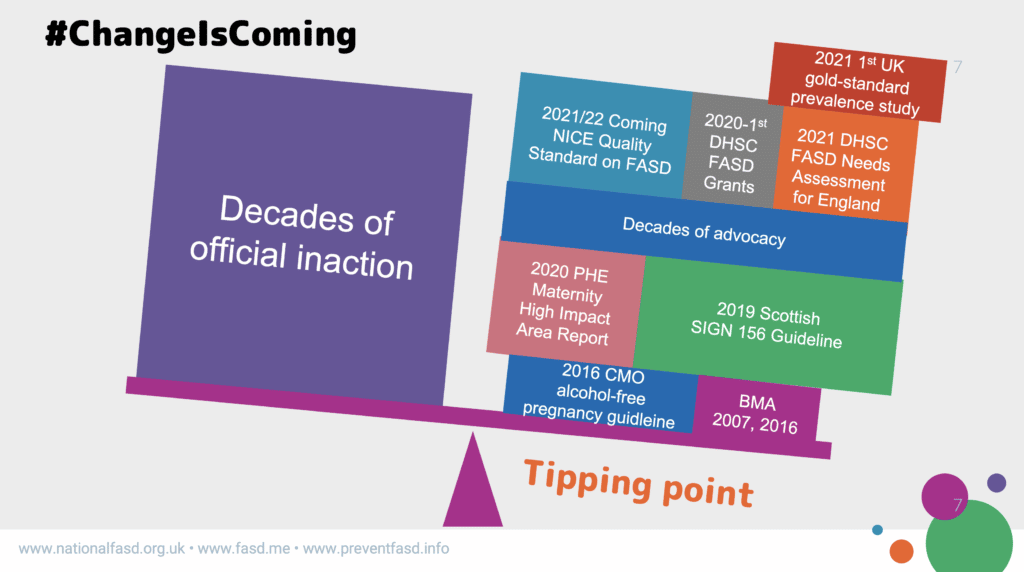
In 2021 alone, we’ve seen some hugely significant and irreversible turning points.
The Department of Health and Social Care (DHSC) unveiled its FASD Health Needs Assessment for England in September at a landmark meeting of the APPG on FASD.
This document highlights:
- a lack of robust prevalence estimates in England;
- the importance of multi-sector working to support individuals through the life course;
- better training and awareness for health professionals;
- better organisation of services to improve accessibility;
- a need to develop innovative approaches to support those living with the condition.
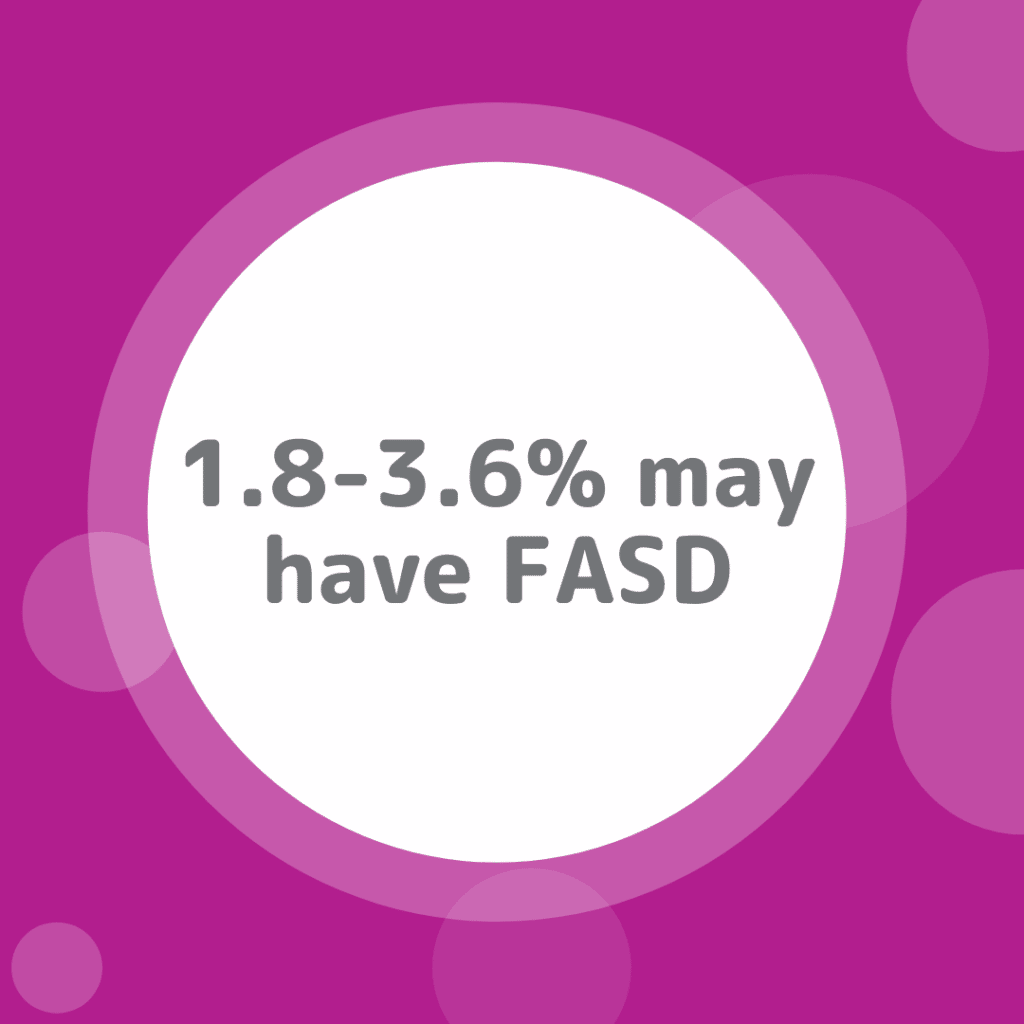
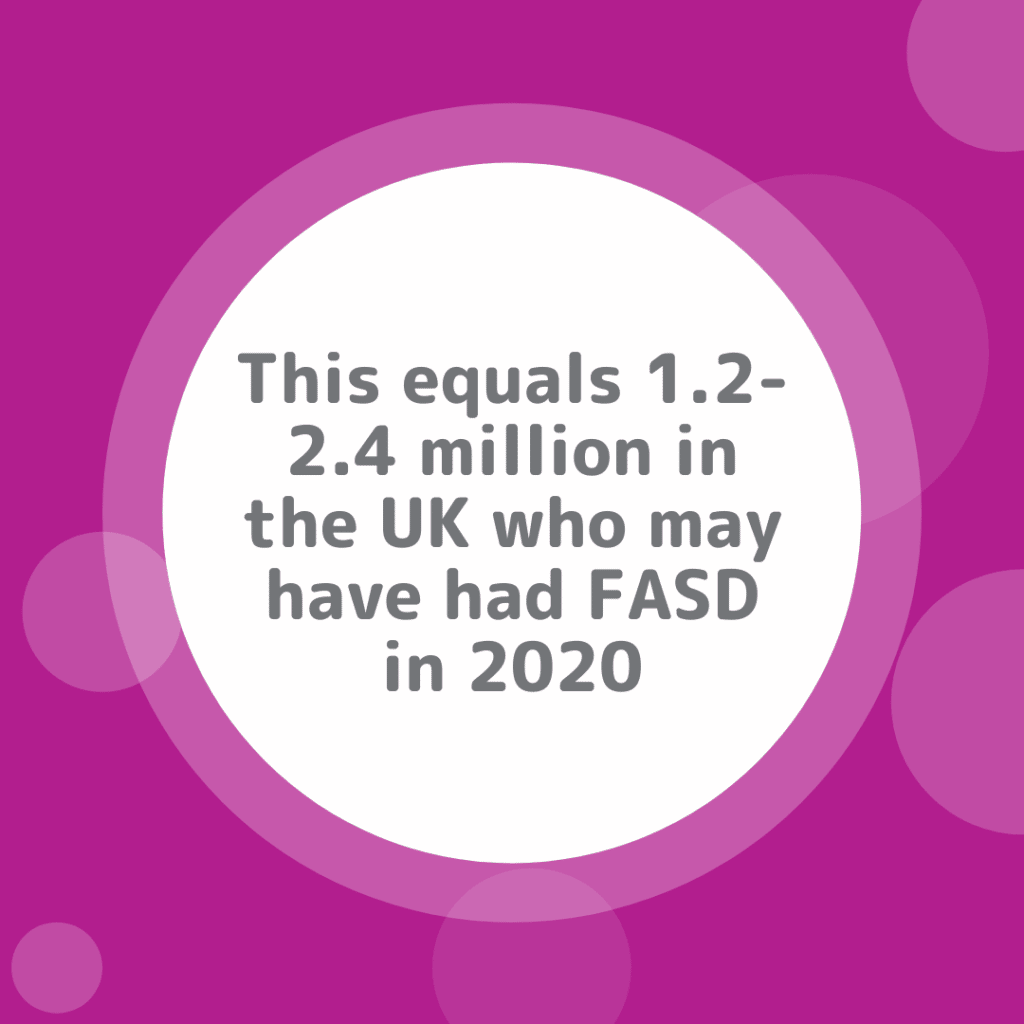
Last year also saw the UK’s first gold standard FASD prevalence study conducted by the University of Salford, which produced data that suggests up to 1.2 – 2.4 million people in the UK could be living with FASD. While a wider UK prevalence study is still needed, this was a much-celebrated step in the right direction.
These leaps and bounds are added to the building weight of progress seen in the last few years, including the CMOs’ 2016 guidance to avoid alcohol in pregnancy, and the 2020 PHE Maternity High Impact Area Report, focused on ‘reducing the incidence of harms caused by alcohol in pregnancy’.
In 2019, Health Improvement Scotland released the SIGN 156 guidelines (accepted by NICE, so these are now also guidelines throughout the UK). SIGN 156 says, “Prenatal alcohol exposure should be actively considered as a possible underlying cause for neurodevelopmental delay, or an unexplained departure from a typical developmental profile.” It lays out diagnostic guidelines and changes the diagnostic terms to FASD with or without sentinel facial features. BOTH diagnoses require evidence of severe impairment in three or more of the identified neurodevelopmental areas of assessment. In other words, this means there is no “mild FASD”.
In addition, last year, in an important case, the Local Government and Social Care Ombudsman raised issue with West Sussex excluding someone with FASD from services for those with “autism or severe learning disabilities”. The ombudsman said, “…the council appears to be gatekeeping access to its services … The council has a duty to ensure there is sufficient educational provision available in its area to meet demand. The lack of suitable placements for the boy in the council’s SEN schools suggests it is not meeting this duty.” This is important because most areas define services this way, and it’s built into the coming Integrated Care Services structure as well. By definition people with FASD with IQs over 70 will be excluded despite their neurodevelopmental challenges.
In 2020-2021, the DHSC also provided its first ever FASD grants, which National FASD and Seashell have used to develop “Resources and Training to Support Children and Young People with FASD” through a cutting-edge partnership. Outcomes include the internationally recognised “Me and My FASD toolkit,” Best Practice in FASD Training Guide, the FASD: Preferred UK Language Guide and expert-reviewed training for a huge range of professionals, including healthcare, social care, and education, as well as a free course for parents and carers!
The tipping point
As more weight is piled on the correct side of the scales, we find ourselves at a point of positive no return, where so much progress has been cemented that it cannot be outweighed by the inaction and stigma of the past.
The draft version has 5 areas (these may change after the consultation process):
- Pregnant women are given advice not to drink alcohol at their first appointment. Advice is non-judgmental and supportive, with follow-up care if needed, such as counselling or help to stop drinking.
- Alcohol-exposed pregnancies will be recorded.
- Children and young people with physical, developmental or behavioural difficulties and probable prenatal alcohol exposure are referred for assessment.
- Neurodevelopmental assessment. Children and young people with confirmed prenatal alcohol exposure or all 3 facial features associated with prenatal alcohol exposure have a neurodevelopmental assessment if there are clinical concerns.
- Management plan. Children and young people with FASD will have a management plan to help coordinate care over a range of healthcare professionals, as well as education and social services.
We have tools in our bag now that have never existed in England before:
If a local authority or trust is not taking FASD seriously, tell them the DHSC is now on record stating, “The government recognises the importance of FASD”.
If a professional says, “There’s no point to diagnosis, it’s just another label,” you can point them toward SIGN 156 and the coming NICE Quality Standard and explain this stance is no longer tenable. Tell them the DHSC has said “Effects of pre-natal alcohol are known to have lifelong consequences.” You can say that each person with FASD deserves attention: “Individuals with FASD are all unique in how the condition affects their cognitive function, and the social impacts it has on them, their families and carers. It is important therefore to take an individualised approach.” Tell them the coming NICE Quality Standard on FASD calls for proper assessments and a care management plan.
In other words, continued inaction is no longer an option.
National FASD looks forward to another year of progress and landmark change, and is committed, as ever, to helping further the cause of greater care and support for people with FASD and their loved ones.
We will be producing materials over coming months to help you use these changes to better support your loved ones. We stand with all our sister organisations in the FASD UK Alliance to ensure people with lived experience are at the core of the change that is coming. #TogetherWeAreStronger